A recent study reported in the NEJM reveals the Dose-Response Curve between hours worked by resident interns and depression prevalence.
This was a huge study, over an 11 year time span, showing a powerful dose response curve between hours worked as a physician and depression prevalence. Said another way: too much time spent as a "provider" inside the healthcare delivery system is bad for your mental health.
I deliberately did not write, "too much time seeing patients" in the sentence above, because we both know the "job" of being an intern or a practicing doctor is so much more complicated than just patient care.
This is a massively important fundamental observation for all practicing physicians and for US national healthcare policy.
Let's take a quick dive into the details.
~~~~~~~~~~~~~~~~~~~~
Stop Physician Burnout, Build Your Ideal Practice
With our 3-Layer Physician Support ECOSYSTEM
Training - Weekly Coaching - A Community of Like-Minded Physicians
Burnout Proof MD - Learn More and Get Started
~~~~~~~~~~~~~~~~~~~~
Let's take a closer look at this important study, then PLEASE LEAVE A COMMENT:
Are you surprised that the relationship is strongly positive?
[Interestingly it is also linear, rather than exponential]What do you think the graph would look like if the research measured burnout rates rather than depression?
Do you think this result would be different if the study subjects were board certified physicians out in practice rather than interns?
Here is the chart that tells the story, then let me give you the study details.
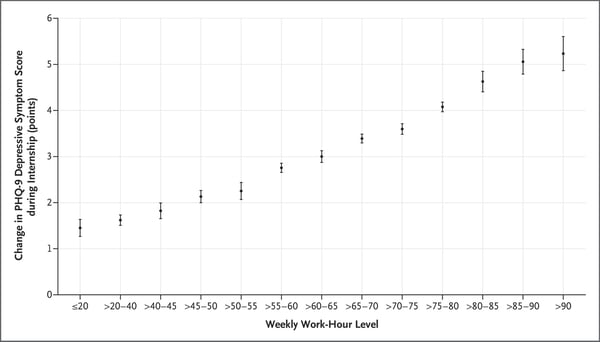
Estimated Mean Change in the PHQ-9 Score for Depressive Symptoms during Physician Internship, According to Weekly Work-Hour Levels, among 17,082 Participants in the Intern Health Study, 2009–2020.
Work Hours and Depression in U.S. First-Year Physicians
Yu Fang, M.S.E.
N Engl J Med 2022; 387:1522-1524
https://www.nejm.org/doi/full/10.1056/NEJMc2210365
Study Design:
(full details below)This was a study of cohorts of US interns recruited in the years 2009 - 2020, a total of 17,082 participants.
- They were surveyed quarterly for depression using the PHQ-9 Patient Health Questionnaire
- And asked how many hours they worked in the preceding week.
What they found:
At baseline, on the first depression screening, fewer than 1 in 20 met the criteria for moderate to severe depression.
Over the course of the internship year, the correlation between hours worked and depression prevalence and severity was revealed. You can see the linear increase in depression scores with hours worked. At over 90 hours/week 1 in 3 met the criteria for depression.
The authors go on to say:
"Reduction in work hours has received only limited mention in the recent recommendations and policy statements addressing clinician well-being.4,5Our findings suggest that limiting the number of hours worked per week by residents has the potential to reduce rates of depression among early-career trainees. "
~~~~~~~~~~~~~~~~~~~~
Walk the Path to your Ideal Practice
Our Certified Physician Burnout Coaches
Are Standing By with One-on-One Support
Schedule Your Free Discovery Session Here
~~~~~~~~~~~~~~~~~~~~
More details from the study:
"We analyzed data from repeated cohorts of U.S. physicians who were recruited annually from April through June during the years 2009 to 2020 to participate in the Intern Health Study (17,082 participants), a national sample of interns (physicians in their first postgraduate year).We assessed depressive symptoms by means of the Patient Health Questionnaire 9-item version (PHQ-93) at baseline (1 to 2 months before the start of the internship) and then quarterly throughout the internship year. On the PHQ-9, depression is categorized as minimal by a score of 0 to 4, mild by a score of 5 to 9, moderate by a score of 10 to 14, moderately severe by a score of 15 to 19, and severe by a score of 20 to 27.
At baseline, we also assessed participants’ demographic characteristics (i.e., age, sex, marital status, and parental status), surgical or nonsurgical specialty, early family environment, personality trait of neuroticism, and history of depression. We gathered data on participant-reported work hours over the preceding week, stressful life events, and medical errors quarterly during the internship."
PLEASE LEAVE A COMMENT:
Are you surprised that the relationship is strongly positive?
[Interestingly it is also linear, rather than exponential]What do you think the graph would look like if the research measured burnout rates rather than depression?
Do you think this result would be different if the study subjects were board certified physicians out in practice rather than interns?

